Are you ready to close care gaps, improve patient outcomes, and reduce costs and administrative burdens? The Veradigm CORE Program offers proactive, clinically-driven services to help health plans and their network providers do just that.
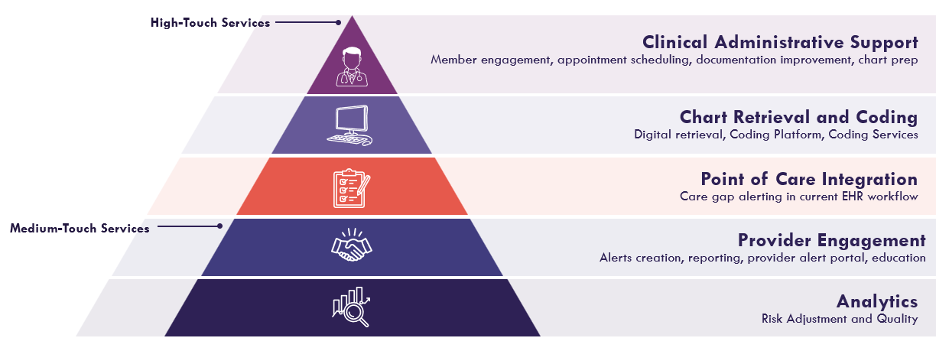
Veradigm leverages digital integration, patented risk adjustment, and quality analytics to streamline provider efforts and drive gap closure. Our CORE services team prioritizes gaps, which helps providers address them quickly without altering existing clinical workflows. This saves time and reduces administrative effort so important care milestones aren’t missed.
A care gap occurs when a patient misses essential healthcare services such as:
Payers can use claims data to identify these missed treatments or conditions that providers should consider. Closing care gaps is paramount because it:
Providers face several hurdles when it comes to closing care gaps. Many are overwhelmed by the number of tools they need to use and the various workflows they must navigate. The impact is significant:
Source: “How EHR Workflows Impact Clinician Experience, Patient Care, and Profitability” an Insiteflow Research Study
Our comprehensive program unlocks the full potential of your health plan by:
*ROI = return on investment
-As of February 2025
-Clients pay for completed gap closure services upon confirmation of documentation in alignment with relevant government reporting standards. Cost per closed gap is a fixed rate, below the amount of the payment premium the health plan will receive as determined by the health profile of its members for Medicare Advantage and Medicaid lines of business. Cost per closed gap does not vary based on documented financial value of the closed gap to the client. Data on file.