Over the last decade, healthcare delivery has changed significantly in the U.S., shifting from a fee-for-service model—reimbursement based on the number of services delivered—to a value-based care model—reimbursement based on quality of care and patient health outcomes.
This shift has significantly changed both healthcare delivery and reimbursement.
The evolving payer provider relationships and its impacts on the healthcare delivery system are core focus areas for Veradigm. That’s why we have compiled this comprehensive guide to payer-provider relationships, including their effects on patient care, how they’re influenced by value-based care, relationship improvement strategies, and more.
Experience Veradigm’s solutions in action.
Who is the provider in healthcare?
Healthcare providers are the individuals or organizations that deliver healthcare services to patients.
Who is the payer in healthcare?
Payers, on the other hand, are organizations such as Medicare, Medicaid, and private insurance companies that process and pay provider claims.
Because they are receiving claims from various providers, payers often have access to a more comprehensive picture of the care a patient receives. In this changing healthcare environment, payers are often responsible for the coordination of patient care.
The payer’s role has evolved to include balancing the costs of care with care quality to achieve the most successful patient outcomes with the least associated expense.
Payers represent the start of the healthcare journey for many patients, frequently providing services such as tools for provider selection or tools to create a more personalized member care experience. Payers also offer a consistent touchpoint throughout the member care experience.
As a result, payers have become a valuable patient resource, able to engage members with health and wellness information that reinforces communications from their healthcare providers and can aid in health-related decision-making.
As the U.S. healthcare system transitions to value-based care, the need for greater payer-provider alignment has become increasingly evident. Payers and providers share the common goals of lowering healthcare costs while improving patient outcomes. If U.S. healthcare is going to achieve high-quality, affordable care, then payers and providers must be able to collaborate on these common goals.
Payer-provider collaboration enables payers and providers to leverage their common goals while taking advantage of each other’s unique strengths in advancing the patient-member experience.
For instance, payers can encourage collaboration with physicians by sharing clinical, quality, and cost-related data. By giving physicians access to the bigger clinical picture for their patients, payers help providers to deliver higher-quality care. Data sharing also enables collaborative accountability: Coordinating quality and outcomes goals encourages payers and providers to adopt mutually agreed-upon strategies for improvement.
Payer-provider collaboration can help physicians reduce their administrative load, benefiting both patients and providers. Streamlining prior authorizations and referrals helps patients access the care they need more quickly while simultaneously giving physicians more time and energy to focus on patient care and improving patient outcomes.
When providers are free to focus on their patients’ individual needs, the entire population benefits—and a healthy population spends less time seeking medical care. This, in turn, reduces the cost burden for payers, helping to create a more effective and efficient healthcare system.
Ultimately, a stronger payer-provider relationship enables a more patient-centric focus, resulting in improved patient outcomes at a lower cost.
Despite the shared goals of improving patient outcomes while managing costs, the road to collaboration is not always smooth.
Payer-provider relations often become strained over issues related to payment and quality of care. Payers are sometimes held responsible for negative patient experiences related to financial challenges caused by provider operational issues; while providers, and the prices they charge, are sometimes blamed for the skyrocketing healthcare costs facing payers.
One key obstacle to establishing a collaborative payer-provider relationship has been physician distrust of payers—the result of decades operating under a system that set the financial interests of payers and providers against one another. A beneficial payer-provider relationship requires physicians and payers to transition from their prior roles to working as partners.
The lack of trust can only be overcome if the insurer actively works to earn providers’ trust. Payers have a wealth of resources they can share with physicians. They can provide data and analytical insights that support the physician’s care strategy; they can offer timely, actionable, and relevant data analytics to help providers to manage patient risk.
Timely sharing of patient-level data and information is key to transforming the payer-provider dynamic and creating a collaborative partnership with the goal of advancing patient-member care.
Another common challenge is the lack of standardization in data collected, formats, systems used, and more.
For instance, CMS, private insurers, and other payers have varied requirements for reporting quality data, which makes reporting quality measures a costly, time-consuming process for healthcare practices. This problem is exacerbated by the need for more standardization among the data elements used for quality measurement and reporting requirements.
Electronic health record (EHR) systems need to be more capable of collecting, aggregating, and correctly formatting data to suit the varying quality reporting requirements. These challenges include accommodating different data formats, analyzing unique populations, and accessing data in disparate storage modalities. Individual risk-adjustment reviews may also require the collection and analysis of specific data elements.
One of the benefits of value-based healthcare is that it provides an environment that encourages payers and providers to establish a mutually supportive and beneficial relationship. This improved payer-provider relationship benefits patient outcomes by enabling providers to focus on addressing patients’ needs. This helps the population as a whole—and a healthier population spends less time seeking care, reducing the overall cost burden on payers and creating a more efficient and effective system overall.
Successful payer-provider collaboration also benefits patient outcomes because most such collaborations involve the use of data analytics tools. This is because data are essential for identifying things such as areas where more preventative care is needed.
Improving payer-provider collaboration can clearly benefit both parties, but navigating the path to an effective relationship can be challenging. These 2 strategies can help payers and providers improve their ability to collaborate on shared goals.
Although both payers and providers operate in the healthcare industry, each frequently has misconceptions about the other’s unique roles, goals, and the pressures they face. Identifying your common goals—such as improving patient health outcomes and controlling costs—can be a starting point. It’s also helpful to identify strengths that each brings to the relationship, as well as weaknesses that the other can help to support. Finding these leverage points can help to build mutual trust.
Sharing clinical and patient information is vital for both payers and providers. Payers require this data to meet their objectives; providers require timely and accurate clinical data in order to deliver the best care to their patients.
However, many health plans currently share patient data using their plan-specific formatting, forcing the provider group to organize and aggregate data from multiple payers or, alternatively, to work with disparate, disjointed data sets. By proactively negotiating with payers, providers can encourage more efficient and effective data sharing. For instance, payers can import data into the provider’s existing data analytics engine. This eliminates the administrative burden of working with multiple data sets or manually aggregating data into a usable format.
Alternatively, providers can negotiate for the use of a payer-agnostic interoperability solution that enables both sides to upload data to a single shared system. By incorporating payer access to patient medical records through a bidirectional interoperability solution, providers can significantly reduce or eliminate the administrative burden associated with sharing patient charts.
Data analytics are a vital component of any data sharing plan, as data analytics are key for measuring the impact of any changes implemented. By negotiating the use of meaningful quality metrics, providers and payers can identify areas of successful change as well as areas potentially needing revision, thus supporting financial sustainability in your relationship.
Providers face significant challenges in adopting value-based care contracts with payers. One common issue is simply practice size, as the majority of primary care physicians work in small physician-owned practices. A recent National Ambulatory Medical Care Survey showed that:
In other words, 65% of primary care visits annually were at small primary care practices with 5 or fewer practitioners.
However, smaller practices frequently lack the resources and/or experience required to effectively implement a value-based care practice model. In a recent survey of solo and smaller group medical practices, respondents listed numerous obstacles to adopting value-based care contracts, such as:
So how can providers—especially providers in smaller medical practices—address these issues? First and most importantly, with preparation. Here are 3 key areas to make sure you prepare before entering negotiations.
Prior to contract negotiations, it’s essential to collect key practice data and financial information. For instance, know the rates charged for your practice’s most commonly billed services. Identify which procedures were most often claimed for reimbursement with each payer and the associated reimbursement rates.
It’s also important to review current payer contracts to better understand which payers currently have the most favorable terms. Some questions to consider include:
It’s critical to familiarize yourself with terms commonly used in value-based care contracts, such as:
It’s essential to familiarize yourself with potentially confusing legal language that sometimes appears in payer contracts, such as:
Before entering contract negotiations, clarify your goals for the negotiation, whether that’s increasing the practice’s net revenue, improving reimbursement accuracy, or putting stricter terms in place for overdue payments. Once you’ve identified and prioritized your goals, be prepared to present your requirements clearly and concisely. You need to be ready to demonstrate that any demands are reasonable—be prepared to respond to potential arguments with data and evidence to support your requirements.
The American Medical Association recently released a comprehensive toolkit to assist private practices with payer negotiations, including a free 2-hour webinar series plus the following publications:
The success of value-based care models is highly dependent on establishing effective and collaborative payer-provider partnerships. However, the increasing use of value-based care models and risk-sharing setups frequently result in increasingly complex payer contracts.
According to a recent report, this increasing complexity is decreasing current payer-provider alignment, rather than improving it.
This report found that only 11% of private payers had a lot of trust in their associated physician groups, while only 6% of providers had a lot of trust in public payers. The lack of confidence seemed tied to communication issues, as most payers and providers reported feelings of disconnect.
Lack of trust combined with limited communications is resulting in misalignment in payers’ and providers’ overall goals for value-based care, which then limits the success of their value-based care initiatives.
Strengthening the payer-provider connection is an essential step if value-based care is to succeed. Fortunately, the right technology, implemented correctly, can be a tremendous help in fostering positive payer-provider relationships.
One key requirement for effective payer-provider collaboration is interoperable data sharing. Sharing data, especially clinical data, is perhaps one of the most critical forms of communication in healthcare. Providers use clinical data for nearly every aspect of provider operations, from making treatment decisions, to tracking and improving patient outcomes, and submitting claims and requests for Prior Authorization. Payers use clinical data as well, for tasks such as determining medical necessity and making prior authorization decisions.
Clinical data exchange is also essential for value-based care, for improving quality scores, and for simplifying risk management. Enabling payer-provider data exchange at the point of care opens the opportunity to proactively identify and communicate information such as gap closure opportunities; it also enables providers to access information to help manage patient care quality.
Traditionally, payer-provider clinical data exchange involved the time-consuming and labor-intensive process of manually tracking down and delivering clinical data, imaging, and other required patient information. Streamlining this process can benefit payers, providers, and patients. The American Journal of Managed Care reports that sharing clinical data can help:
Effective clinical data exchange can deliver actionable information to providers, helping them to make more informed healthcare decisions for patients. CMS states that improved data-sharing can help drive better patient care by better informing decision-making for both patients and providers. More effective clinical data exchange also makes it easier for providers to review patient data in a timely manner, facilitating care management decisions and accelerating payers’ ability to make medical necessity and prior authorization decisions. It also helps to close care gaps because patients can be treated more quickly, driving improved patient outcomes.
Healthcare data exchange is critical for controlling healthcare costs. It does so, in part, by decreasing the administrative burden on both healthcare providers and payers. However, sharing healthcare data also means payers and providers can work together, providing proactive healthcare to patients and increasing care coordination—both of which can help to decrease healthcare costs.
Finally, effective data change contributes to lowered costs by making the process more efficient.
By leveraging technology solutions, payers and providers can improve clinical data exchange, facilitate the prior authorization process, identify and exchange information regarding gaps in care, and more. However, for a data exchange solution to be useful, it needs to be simple and convenient. It also needs to occur without disrupting the provider’s workflow. To maximize provider utilization, the solution should ideally fit into the normal process of documenting patient visits.
Improving payer-provider communications is a focus area for Veradigm, which is why we offer a number of solutions that can help streamline payer-provider interactions.
Veradigm Payer Insights is a dynamic solution that allows payers to deliver care gap alerts to their providers, within specific patients’ EHR records, as part of the provider’s existing clinical workflow.
Previously, identifying potential patient gaps in care required providers to proactively log into payer portals or other outside sites. However, if documentation of gaps in care is not accessible at the point of care, during the provider’s normal patient visit workflow, the potential for that information to positively impact patient care is greatly reduced. Veradigm Payer Insights reduces provider abrasion by delivering a free and easy-to-use solution to this challenge.
Leveraging the Veradigm Network, Veradigm Payer Insights enables large-scale, bi-directional interoperability between payers and providers. Payers can identify and access additional gaps in care using their providers’ EHR data, based on their specific criteria. They can then generate seamless gap in care alerts within the EHR workflow. Alerts contain relevant, patient-specific information for the provider to evaluate and address with the patient.
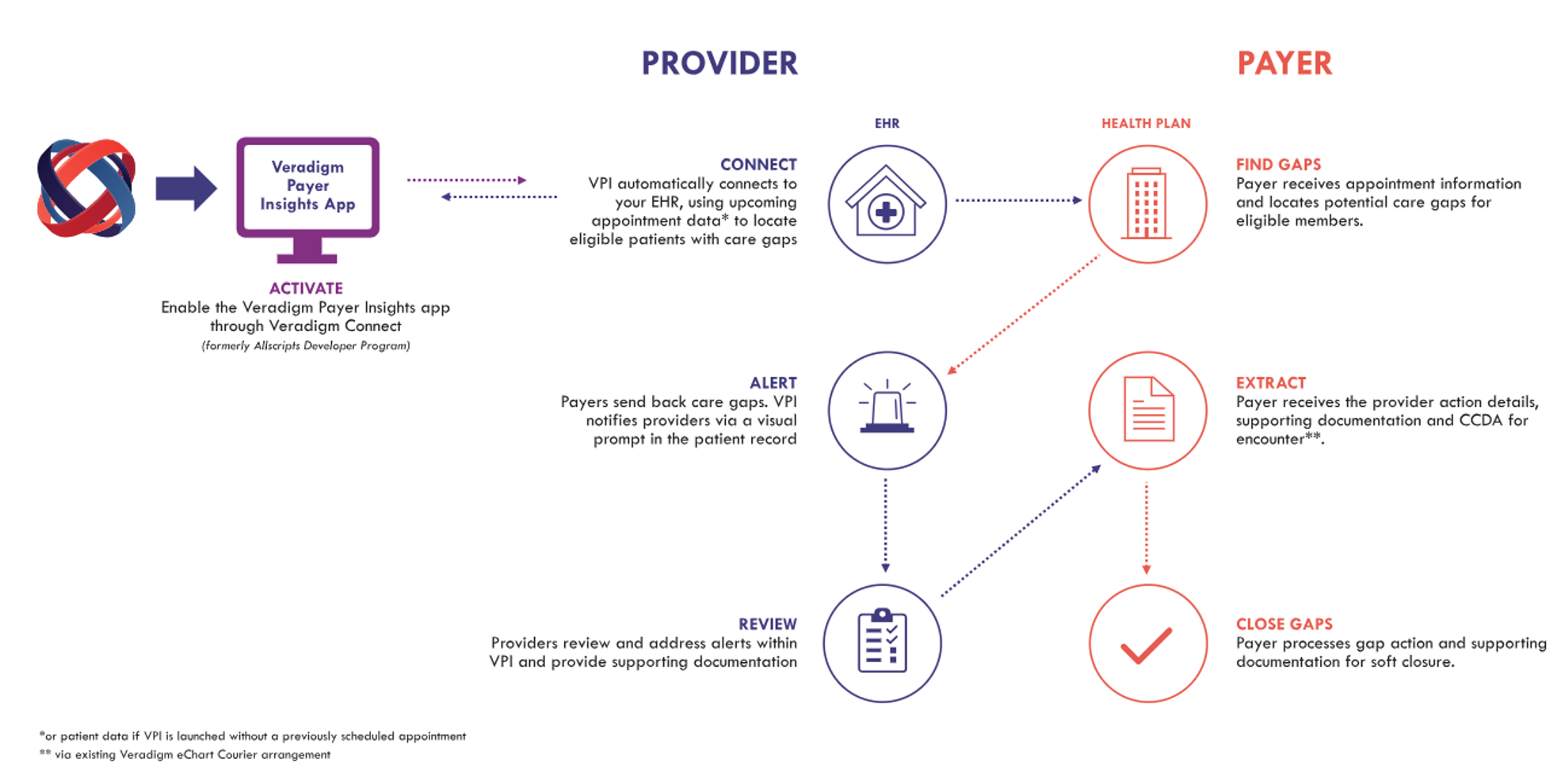
With Veradigm Payer Insights, payers and providers can collaborate to help minimize risk and improve patient outcomes.
eChart Courier facilitates payer-provider collaboration by streamlining the medical chart retrieval process. This solution saves time, cost, and resources by enabling the electronic retrieval of patient charts.
Manual chart retrieval is a time-consuming process that diverts resources that could be better used to support patients.
eChart Courier automates medical chart retrieval, enabling healthcare providers to share patients’ medical records with payers seamlessly and securely. eChart Courier operates through the practice’s EHR system, increasing efficiency and allowing chart access without changing the provider workflow. Information is then delivered in a secure, HIPAA-compliant fashion.
Veradigm Collaborate is part of a suite of solutions designed to optimize payer-provider interactions and make gap closure efforts as efficient and effective as possible. Veradigm Collaborate enables more efficient payer-provider communication, minimizing provider abrasion and alert fatigue. It allows consolidation of provider alerts for risk adjustment, quality, and pharmacy opportunities. Customizable prioritization algorithms enable delivery of only the highest confidence level alerts. Payers can also configure multiple types of content for provider notifications for maximum flexibility.
Veradigm Collaborate helps payers identify the best opportunities for provider engagement. Flexible dashboards help users identify groups, providers, and members with the greatest overall impact, to help prioritize focus areas. Data from multiple risk adjustment and quality sources are consolidated and aggregated into single-member alerts and limited to one alert per member to minimize provider burden.
Veradigm Collaborate also encourages provider collaboration and engagement by delivering value at multiple levels:
The payer-provider relationship went through significant changes in 2023, and this trend is expected to continue in 2024 as the shift to value-based care grows. Some of these anticipated trends include:
Payer-provider relationships have long been extremely complex: The provider may be dealing with Medicare, Medicare Advantage, Medicaid, self-pay, direct-to-employer, and multiple commercial insurers—each with their own requirements for data collection and quality measurement. With providers contracting with multiple public, private, and self-funded payers, data collection requirements alone can become overwhelming. The costs and administrative burden have been well documented, with studies showing a potential savings of as much as $350 billion by implementing a simplified financial system.
Rapidly evolving healthcare policies can make these relationships even more demanding, as both payer and provider organizations face new territories stemming from changes in healthcare policy requirements related to health equity drivers, social risk, value-based care imperatives, and more.
Let’s look at some of the more notable healthcare policy changes and how they affect payer-provider dynamics.
The shift to value-based healthcare has made payer-provider collaboration essential—and value-based healthcare is at the root of many of the current changes in healthcare policy.
Value-based care, with its requirement for greater payer-provider partnership, also requires improved payer-provider communication of clinical and patient-related data. Increased interoperability would address this need, enabling increased data exchange and increasing opportunities for payers to support and collaborate with their providers.
CMS’s Advancing Interoperability and Improving Prior Authorization Processes Proposed Rule (CMS-057-P), currently under evaluation for inclusion in a final rule, addresses this need for increased interoperability to facilitate payer-provider data exchange—and it is also extremely likely to increase the need for increased payer-provider collaboration. The proposed rule:
Value-based care also makes it critical for patient data to reach providers in a timely manner, encouraging ever-closer payer-provider collaboration. Only with a close payer-provider relationship can a true partnership be formed, and only with a true partnership can stakeholders implement a proactive approach to patient care.
Not only is it critical to be able to deliver key patient data to providers at the point of care, but that data needs to be in a useful form. It also needs to reach providers while they are actually seeing their patients, when they are most likely to be able to use it to meaningly affect the patient’s care.
Veradigm is dedicated to simplifying and streamlining payer-provider relationships. Our unique portfolio of collaborative solutions facilitates data exchange, enhances vital payer-provider communications, and more. Veradigm’s tools can support your value-based care initiatives in an ever-evolving healthcare environment.
With innovative, insightful solutions, Veradigm is poised to help health plans, healthcare providers, and the patients they serve to improve patient outcomes, minimize patient risk, and streamline payer-provider collaboration.
Discover Veradigm Payer Insights, the solution enabling seamless, efficient patient care by bridging the communication gap between payers and providers.
Read morePayer-Provider collaboration is unlikely to succeed if the process is complicated & resource intensive. Here are solutions that won’t disrupt provider workflow.
Read moreLearn how a streamlined payer-provider clinical data exchange can improve care coordination & patient outcomes while lowering healthcare costs.
Read moreExplore how Veradigm is pioneering the integration of AI in healthcare, reshaping the landscape for providers, payers, and biopharma. Learn about an AI-driven future.
Read moreThere is significant opportunity to reduce waste in the healthcare ecosystem by automating manual processes with savings opportunities for both payers and HCPs. Automating manual processes also improve payer-provider relationships and enhances member satisfaction.
Read moreHealth plans of all sizes need to start thinking now about how to prepare for their path toward clinical interoperability.
Read moreMedical record retrievals provide data for calculating HEDIS measures, CMS Stars Ratings, risk adjustment reviews, and more. Read why providers should care.
Read moreExplore Veradigm's holistic approach to payer-provider relationships and healthcare delivery through its innovative Payer Solutions.
Read moreEffective information exchange between health plans and providers, where clinical data and insights are shared, can have a significant impact on the quality of care delivered.
Read moreDiscover how payers can lay the foundation for the next phase of healthcare interoperability by focusing on tools that facilitate clinical data exchange.
Read moreThe Veradigm Value-Based Analytics solution provides analytics and insights to identify targets for improvement for value-based contracts and programs.
Read moreAs part of Veradigm, Koha Health’s services now include advanced support for managing staff, streamlining workflows, ensuring medical coding accuracy, insurance claims submission, and comprehensive reporting. This integration is designed to leverage your existing technology investments and drive meaningful improvements that impact your bottom line. With Veradigm, you gain access to an expanded suite of tools and resources that build a strong foundation for future success. From efficient revenue cycle management to enhanced patient care, Veradigm is committed to supporting your goals now and into the future.
Allscripts transitioned its solutions to the Veradigm brand, including electronic health records, practice management systems, and patient engagement platforms in 2022. Veradigm is a healthcare technology company that drives value through its unique combination of platforms, data, expertise, connectivity, and scale. The Veradigm Network features a dynamic community of solutions and partners providing advanced insights, technology, and data-driven solutions for the healthcare provider, payer, and life science markets.
Former Pulse8 solutions are now part of the Veradigm Payer Analytics portfolio. In addition to delivering complete visibility into the efficacy of your Risk Adjustment, Quality Management, and Pharmacy programs through former Pulse8 solutions like Calcul8, Qualit8, and others, Veradigm offers a broad range of solutions to help Payers meet their goals for supporting high-quality, cost-effective patient care.
Babel Health solutions are now part of Veradigm Payer Analytics, with enhanced Risk Adjustment (RA) submission workflow creating an end-to-end solution for regional health plans and payers. With Veradigm, Babel clients can receive enhanced support with the ability to leverage a truly end-to-end suite of products and solutions. From RA and Quality analytics and reporting, provider engagement tools, and comprehensive submissions solutions, Veradigm is positioned to support your goals now and in the future.
Evalytica platform is now part of the Veradigm Network and is known as Veradigm Real-World Evidence (RWE) Analytics Platform , a powerful self-service analytic platform. This transition allows for the advancement of our RWE Analytics technology, expansion of the platform and improvement of its capabilities, functionality, and reach.